Terbium-161
Combines β– emission with low-energy Auger and conversion electrons.
Produced with high radionuclidic purity.
Tailored to ensure alignment.
What is Terbium-161?
Terbium-161 (Tb-161) is one of the radioactive isotopes of the rare earth element terbium. This medical isotope has recently been identified as a potential treatment for metastasized prostate cancer and neuroendocrine tumors.
This valuable radioisotope is irradiated in batches in our nuclear facilities.
Contact
More information about Terbium-161?

Marjolijn Droog
Business manager Isotopes

Specifications Terbium-161
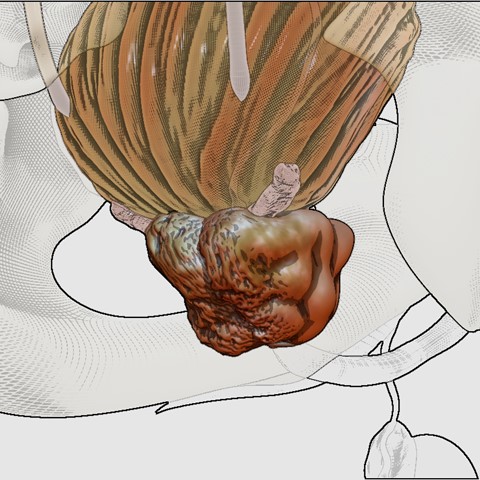
Tb-161 undergoes beta-minus decay with a half-life of 6.953(2) days, transforming into stable Dysprosium-161 (Dy-161). Its half-life is slightly—less than 5%—longer than that of Lutetium-177 (Lu-177). As a beta-emitter is only deposits its energy within a short range, decreasing collateral damaging effects to normal tissues.
In addition to beta particles, Tb-161 emits a significant number of low-energy conversion electrons and Auger electrons, resulting in the release of approximately 2.27 electrons per decay with energies exceeding 3 keV. Furthermore, Tb-161 emits both gamma and X-rays, most notably with a 43.1(5)% emission around 48 keV (±10%) and a 10.3(2)% emission at 74.6 keV. These photon energies make Tb-161 well-suited for SPECT imaging.
Terbium-161 could be a substitute of Lu-177 PSMA for radionuclide therapy of metastasized castration-resistant prostate cancer (mCRPC). The properties of Tb-161 are similar to those of Lu-177. It is believed, however, that the co-emission of conversion and Auger electrons make terbium-161 superior. These short-ranged electrons may effectively eliminate microscopic metastases that are not even visible on a PET image, but responsible for relapse and metastatic spread.
Similar to other recently introduced therapeutic radionuclides, such as Actinium-225 (Ac-225) and Lead-212 (Pb-212), Tb-161 and Lu-177 undergo decay to stable isotopes (Dysprosium-161 and Hafnium-177, respectively), thereby avoiding the risk associated with particle-emitting daughter products.
How is it made?
NRG|PALLAS produces Tb-161 in our High Flux Reactor (HFR) through neutron irradiation of enriched Gadolinium-160 (Gd-160). Upon capturing a neutron, Gd-160 is converted into Gd-161, an unstable isotope that subsequently undergoes beta decay. This process results in the transformation of Tb-161, accompanied by the emission of beta particles and gamma radiation.
The key reaction can be represented as follows:
Gd-160 (n,γ) Gd-161 -> Tb-161 + β- + γ
The produced Tb-161 should be separated from the Gd160, purified and processed to meet the required quality and safety standards before it can be used in medical settings.

What is it used for?
Tb-161, one of four medically relevant terbium isotopes, is considered a natural successor to Lu-177 due to their closely related chemical and nuclear characteristics. Compared to Lu-177, Tb-161 offers enhanced therapeutic potential by delivering a higher localized radiation dose, particularly within micrometer-scale distances—more than doubling the dose per decay in some cases. This advantage has been demonstrated in various preclinical studies using different radiopharmaceuticals. In addition, Tb-161 emits photons with distinct energies from Lu-177, allowing for dual-radionuclide SPECT imaging. Clinical imaging protocols have already been proposed, and first-in-human use of Tb-161-DOTATOC—including SPECT/CT imaging up to 113 hours post-injection—has been reported. Beyond therapy and diagnostics, Tb-161 can also serve as a source for Mößbauer spectroscopy, enabling precise characterization of terbium’s chemical state in solid or frozen biological samples.

