Promising results in using biokinetic model to predict behavior of nuclear medicine in the body
Promising results in using biokinetic model to predict behavior of nuclear medicine in the body
26 March 2022
In order to predict the behavior of nuclear medicine in the body after administration, Ramona Bouwman, consultant radiation protection at NRG, has been developing a biokinetic model to do just that. The model has been tested using patient data of the Netherlands Cancer Institute and the results are promising.

Predicting what happens in the body during treatment
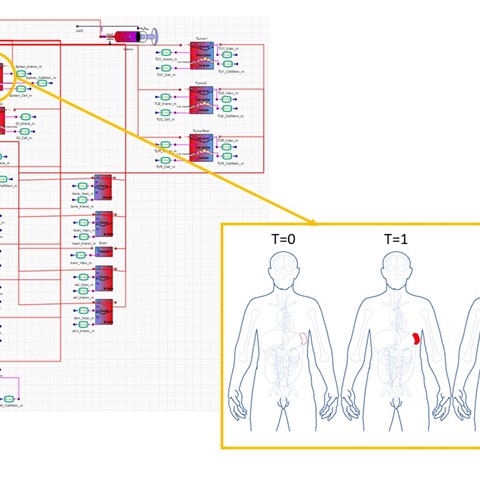
Bouwman has a background in applied physics and has been working on this model since 2019. A biokinetic model is a set of mathematical functions that describe the time-dependent behavior of materials that enter the body intended or unintentionally. They are used to predict the time-dependent distribution of materials in the body up to sub-cell level and their elimination rates along specific excretion pathways. “These models predict what happens in the body during treatment, taking into account the individual characteristics of a patient and the properties of the medicine or radionuclide. This allows a physician to optimize treatment of cancer, for instance, or help in the development of new medicine. An extra advantage of the latter is that this model might reduce animal testing or the length of clinical trials in the future”, Bouwman says.
Limiting damage and reducing side effects
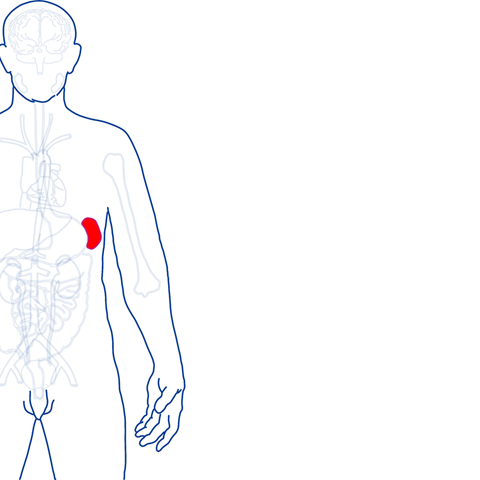
The model is being developed on the software platform PhysPK© and shows how specific tumors and organs absorb the administered nuclear drug, which consists of a molecule (peptide), combined with a medical isotope (nuclear medicine). This treatment is called peptide receptor radionuclide therapy, or PRRT. “In the tumor cells there are specific receptors that bind to administrated peptides. Via this receptor the peptides with a medical isotope will be absorbed by the cell, where the radioactive component will damage the tumor cells. Bouwman explains: “It is important that during this process, the radioactive decay takes place as much as possible in tumor cells rather than near healthy cells. This will limit the damage to other tissue and reduce potential side effects of the treatment.”
It also takes into account the personal characteristics of the patient, enabling it to determine the right dosage for every patient to achieve the optimal treatment. Bouwman: “Every patient is different. That is why it is so valuable that we can also enter the personal characteristics of the patient into the model.”
The model can then be used to predict the effect of the treatment and help work towards ‘personalised medicine’, a treatment tailored to the individual. Furthermore, biokinetic computer simulations will support the research of new nuclear medicine in the future. “The computer model can predict the effects of the new drug on the body. It can possibly partially replace testing on humans and animals.”
“Once the model is fully functional, we can optimize treatment of the patient and reach our ultimate goal. Fight the tumor, while minimizing damage”
Promising results
Before the model can actually be implemented in hospitals and in research, further research is necessary. “Everything you model, you have to validate in real life. To compare the prediction of the model with real patient data, I have received patient data from the Netherlands Cancer Institute (NKI) and applied this data to the model. We have now been able to complete the model and test the accuracy of the predictions. We still have some steps to take and parameters to tune to get all the predictions right. But the results so far have been very hopeful.”
According to Bouwman, it will probably be another 10-15 years before the model can be used in hospitals on a large scale to help administer a tailor-made radionuclide therapy. Other factors still need to be included, like expected damage to organs at risk like the kidneys and tumors with different characteristics. “Once the model is fully functional, we can optimize treatment of the patient and reach our ultimate goal. Fight the tumor, while minimising damage.”
More information?
Do you wish to learn more on nuclear medicine and how FIELD-LAB can help you? Get in touch with us!

